
Why is sex painful? pt. II: Common causes of “superficial” dyspareunia, pain felt in the vulva and/or the entrance of the vagina
By Allison Danish, MPH
Wondering why you’re “OW”ing instead of “OH”ing? Welcome to the second installment on the “why” behind dyspareunia, or painful sex. Why is Sex Painful? Pt. I discusses deep dyspareunia, pain felt deeper in the body. In this article we’re talking “superficial” dyspareunia, pain felt in the vulva and/or the entrance of the vagina. Let’s get to it.
Vaginismus
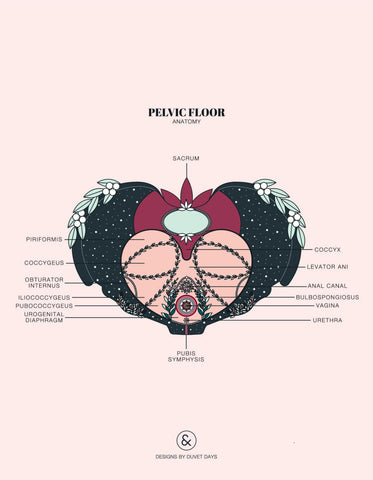
Vaginismus, also now referred to as genito-pelvic pain/penetration disorder, is when the pelvic floor muscles involuntarily tense up, making penetration impossible or very painful. When penetration is impending, anticipation of pain can cause the vagina to pull a Gandalf and say, “You shall not pass!” Many people say this feels like “hitting a wall.” Attempting penetration when these muscles are tensed can result in pain that is very real (not just in your head!), reinforcing those initial fears that caused the muscles to contract in the first place.
Vaginismus can rear its head anytime. For some, it starts with difficulty inserting a tampon or even a pinky finger. For others, it happens the first time penetrative sex is attempted. It can develop later in life too. Some people can have pleasant experiences with penetrative sex, and then experience this tensing and subsequent pain later in life.
Currently, it’s thought that vaginismus heavily involves the fear response. The pervasive belief that “the first time” is supposed to be painful, strict moral beliefs about sex, past sexual trauma, anxiety, and current abuse can all be causes. Beliefs and experiences heavily impact our brains, and can create fear and apprehension that result in very real physical responses. When those physical responses make sex painful, it is stressful! It is scary. The brain takes note that it was right to be fearful because that was painful, and the cycle continues. While disrupting that cycle can be difficult, it’s certainly possible to retrain our experience.
Treatment options include sex therapy, pelvic floor physical therapy, a vibrating entry pain massager like Kiwi, programs like HelloGina, and vaginal dilation (with dilators like these from Soul Source).
Vulvodynia
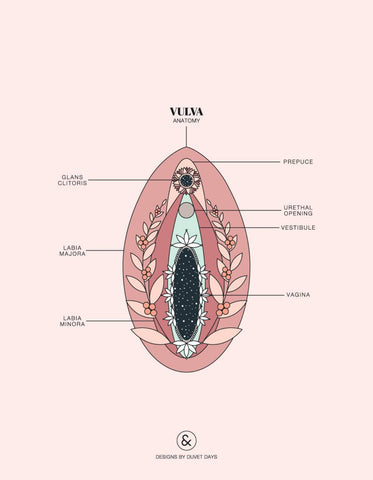
Vulvodynia is chronic, unexplained vulvar pain (though there is often an explanation with further investigation). It is most commonly localized (pain only occurs at one spot on the vulva), but can also be generalized (occurring at more than one spot at different times). This vulvar pain can begin during/after the first attempt at vaginal penetration (primary vulvodynia) or can develop later on in life after having had pain-free sex (secondary vulvodynia). The onset of vulvodynia is most common in 18–25 year olds in the United States, leaving the vulva feeling sting-y, irritated, or raw. Those with vulvodynia may also feel burning, throbbing, or aching sensations, soreness, and swelling. This pain can be spontaneous or may be provoked by touch (from sexy touching, to less-sexy pelvic exam touching, to a pair of tight pants).
There’s no one cause of vulvodynia, but some possible culprits include infections, inflammation, nerve injury, and pelvic floor dysfunction. Vulvodynia can cause superficial dyspareunia because the vulva is where a lot of the magic happens! Touch isn’t exactly welcome when the vulva is tender or actively in pain. But hey — you’re certainly not alone, my friend. Vulvodynia affects up to 16% of vulva-havers.
Pelvic floor physical therapy is a common treatment option for vulvodynia, as well as topical medications and “pain-blockers” that can relieve discomfort. Other treatment options range from antidepressants and anti-seizure medications to more alternative methods of treatment like acupuncture and CBD products. Lifestyle changes like avoiding bike riding and tight-fitting pants can be useful too — plus there’s this nifty little device called the Sili Saddle that can be used as a cold or hot pack for the vulva and Private Packs is an ice pack specifically made for vulvar pain. Kiwi may also be a helpful tool for managing vulvodynia caused by pelvic floor dysfunction!
Vestibulodynia
Vestibulodynia, often thought of as a subtype of vulvodynia, is chronic pain in and around the vestibule, the entrance to the vagina. The vagina’s lobby, if you will. Pain can be brought on by gentle touches, prolonged sitting, and penetration (be it a penis, a dildo, or a tampon).
Vestibulodynia causes painful sex because it can make any kind of penetration uncomfortable. While penetration might not always be a comfy option, this creates an excellent opportunity to explore the rest of the body! Check out these tips for non-penetrative sex.
While vestibulodynia as a diagnosis is vestibular pain without discernible cause, there are indeed causes! Check out this article on the most common causes of provoked vestibulodynia (or "entry pain") here.
Vaginal dryness
Vaginal dryness or insufficient lubrication can happen for a lot of reasons!
Lack of arousal:
- The body’s natural homegrown lube mostly comes from the walls of the vagina, though the Bartholin’s glands and Skene’s glands play a role as well. Maybe a little more foreplay, taking a different approach to foreplay, or a change in environment is needed to make things juicier.
Low estrogen:
- Estrogen increases blood flow to the vagina and helps keep it moist! Low estrogen can be caused by menopause, cancer therapy, childbirth, breastfeeding, anti-estrogen medications, and having the ovaries removed or being born without them.
Testosterone:
- Testosterone helps make red blood cells and can be converted to estrogen. When T is low, there’s less blood flow and less estrogen — leading to potential dryness. Because testosterone is produced in the ovaries and adrenal glands, low T can be caused by menopause and aging, the removal of ovaries, or problems with the adrenal glands.
- Having a lot of circulating testosterone—for instance, if you're a trans man taking testosterone—can also be a cause of dryness and atrophy of the vaginal tissue—which, again, can make penetration uncomfy! Current treatment strategies suggest that using a local estrogen cream can help with symptoms, but won't interfere with the desired effects of testosterone treatment.
Gender affirmation surgery:
- Some gender-affirming vaginoplasty methods result in neovaginas that are not self-lubricating, so lube is needed to make friction go smoothly and painlessly. Vaginal dilation is also a required part of maintaining the depth and width of the vagina post-surgery.
Douching:
- The vagina is a self-cleaning oven, and a darn good one, so douching is unnecessary and in some cases harmful. Douching can cause vaginal dryness because it disrupts the vagina’s natural balance of good bacteria that maintain its acidic environment.
Sjogren’s syndrome:
- This is a relatively common autoimmune disease that causes dryness in the eyes, mouth, and vagina.
High osmolality lube:
- Some lubes have more dissolved particles (like sodium and potassium) in their liquid than others. This makes the lube hyperosmolar or more concentrated. Our cells also have fluid and particles in them, and they long for harmony (or what the kids call homeostasis). So, if the cells that make up the vaginal walls have fewer particles (are less concentrated) than the lube you’re using, those vaginal cells will want to give up some of their fluid to dilute the lube so the liquid inside and outside the cells have the same concentration. Unfortunately, this can leave the vagina high and dry — literally. There are a lot of lubes on the market, and it can be hard to decide. We highly recommend Oh Naturale organic aloe-based lubricant!
Infection
Infections, both sexually transmitted and otherwise, can cause itching, burning, pain, and general discomfort that can make sex an uncomfortable experience.
- Sexually transmitted infections (STIs): STIs that can cause superficial dyspareunia include genital herpes (sores), genital warts, and trichomoniasis (a parasitic infection).
- Household infections: Other infections that are not necessarily sexually transmitted that can make sex uncomfortable are urinary tract infections, bacterial vaginosis (vaginal bacteria overgrowth), and yeast infections (vaginal yeast overgrowth).
Autoimmune and inflammatory diseases
Certain autoimmune diseases and diseases that cause inflammation, the swelling and often reddening of tissue, can make sex painful. These include:
Interstitial cystitis (IC):
- IC is a condition of unknown origin in which there is pain and what feels like pressure around the bladder, often accompanied by a frequent and urgent need to pee. It may feel like you have a bladder infection when there is, in fact, no infection. It can cause superficial dyspareunia because IC can cause vaginal burning as well as vulvar pain.
Systemic sclerosis:
- This is an autoimmune disorder that affects the skin and connective tissue because too much collagen is being produced. It may tighten the vagina’s lobby (the vestibule, if you’ll recall) and decrease lubrication, both of which can lead to superficial dyspareunia.
Vulvar Crohn’s disease:
- Crohn’s disease is an inflammatory bowel disease that can also affect other regions of the body around the bowel, including the vulva. Inflammation, as well as the development of ulcers and abscesses, is possible and can cause painful sex.
Desquamative inflammatory vaginitis:
- Ah, yes. Another scary-sounding term. Unfortunately, this one doesn’t even have an acronym. Desquamative inflammatory vaginitis is the inflammation of the vaginal lining, and has no clear cause. This inflammation can cause itching and irritation that can cause penetration to be painful, and is accompanied by abnormal vaginal discharge.
Skin conditions
There are several non-contagious skin conditions that can cause superficial dyspareunia.
Dermatitis:
- The vulva is pretty sensitive and can be irritated by things like soaps, laundry detergents, and menstrual products like pads and tampons. This irritation can cause itching and burning, a raw or damp feeling, and skin thickening. In advanced cases, the vulva can become so irritated that penetrative sex and tampon insertion can be painful.
Lichen sclerosus:
- Lichen (pronounced liken or Lycan if you also got too into the Underworld movies) sclerosus is a skin condition of unknown origin, though hormones and the immune response have been implicated. It’s characterized by thin, white patches of skin most often on the vulva, and is most common postmenopause. These patches can cause itching, discomfort, easy bruising and tearing, and can sometimes cause painful lesions. Discomfort and pain caused by the patches, lesions, or scarring in severe cases can make sexual activity unpleasant.
Lichen planus:
- Lichen planus is a rare inflammatory disease with no known cause that causes an itching or burning rash or purple lesions. It can pop up on the skin, inside the mouth, and on the genitals, and is most common in those who are menopausal or postmenopausal. Lichen planus can make sex painful because the rash and/or lesions can cause itching, burning, and pain, and can also cause scarring that can make changes to the vulva that make sex less pleasurable or painful (for instance tightening the vaginal opening). Lichen planus can also result in a shortened or narrowed vagina by the eroding the vaginal walls, making penetration painful.
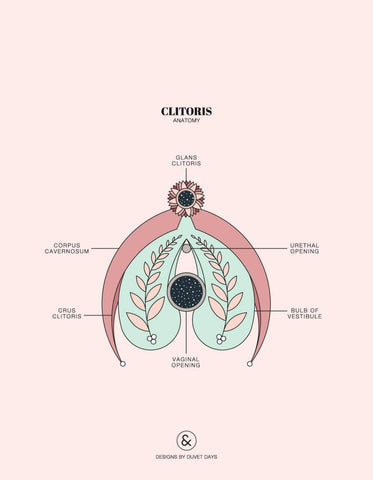
Anatomical
Sometimes the way the vulva and vagina are shaped can lead to superficial dyspareunia. Some people are born with either a partially or completely imperforate hymen, meaning the thin membrane around the vaginal opening called the hymen partially or completely covers the vestibule, which can make penetration very painful. Vaginal agenesis, having either a partial or absent vagina, can make penetrative sex painful or impossible without treatment. Scarring from surgery, tearing during childbirth, sexual trauma, or other vulvar/vaginal conditions can also cause painful sex because it can change or shrink the inner lips of the vulva, cover the clitoris, and narrow the vaginal opening.
Cancer
Vulvar and vaginal cancers can cause itching, pain, burning, and sometimes open sores that can make penetrative sex uncomfortable or painful.
Superficial dyspareunia, and painful sex in general, has a long list of potential causes, so it’s no wonder nearly 75% of people with vaginas will experience painful penetrative sex during their lifetime.
A lot of the sources of dyspareunia, both deep and superficial, are still in a Black Box; we just don’t know why they happen. However, there’s a lot of mounting passion and momentum in the field of sexual health. The number of new scientific articles on sexual health from this decade is more than double that of the last. Educators, therapists, coaches, researchers, and healthtech companies are growing in number, working hard to help you seek pleasure and alleviate pain.
Artwork: © Designs by Duvet Days / All Rights Reserved
