
Why is sex painful? pt. I: Common reasons why you might be feeling deep pelvic pain during or after sex
By Allison Danish, MPH
Painful sex and tootsie pops have one unlikely thing in common: they come in many flavors. Unwelcome vulvar pains, pains in and near the vaginal opening, and, of course, pain that’s felt deeper inside the body. That deep pain is called deep dyspareunia. Under the broader umbrella term describing painful sex—dyspareunia— deep dyspareunia can be stabbing, cramping, or shooting pain felt in the vaginal canal or pelvic area during or after penetrative sex. Mysterious, frustrating, and, above all, painful, it has many causes. Some of these conditions may coexist, while in other cases none of these diagnoses are the answer to this question: why is sex deeply painful?
Below are the most common reasons why you might be feeling deep pelvic pain during or after sex.
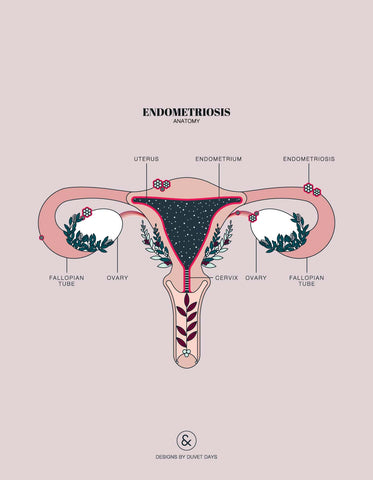
Endometriosis
Endometriosis is a condition in which tissue very similar to the endometrium (the wallpaper of the uterus) starts growing outside the uterus (like on the fallopian tubes and the bowels). It can affect anyone with a uterus, but can persist even after a hysterectomy. Affecting over 11% of uterus-havers in the US, it is most common among those in their 30s and 40s (however this age range is likely due to the delay in diagnosis rather than the age of development).
Endo is characterized by really painful periods, sometimes with heavy flow and bleeding between periods. It can also make sex, peeing, and bowel movements painful, and may lead to infertility. Because urination and bowel movements can be painful with endo, many patients are diagnosed with irritable bowel syndrome/bowel dysfunction or interstitial cystitis. This can be a misdiagnosis, or a patient may have both conditions. Check out the 6 most common signs you might have endometriosis here.
Endometriosis most commonly causes deep dyspareunia when that rogue tissue sticks the back of the vagina to the front of the rectum. Sex tends to squish the pelvic organs around, so that tissue may stretch or tear, causing pain. This can also make tenting (the lengthening of the vagina during arousal) uncomfortable. Read up on other reasons why endo can cause painful sex here.
There is still much to learn about endometriosis, but as awareness grows, the need for more research and treatment options grows. In the meantime, it is still entirely possible to have a fulfilling sex life. Currently, surgery is the most common practice for relieving symptoms by removing endometrial lesions that cause pain. Most people require a multidisciplinary treatment approach that can include surgery, but also treatments like physical therapy, medications (often hormones), and acupuncture. Tools like Ohnut can also help relieve pain and promote pleasure in the bedroom. In fact, Ohnut has been scientifically proven to be an effective at-home strategy for managing pain during sex for people with endo!
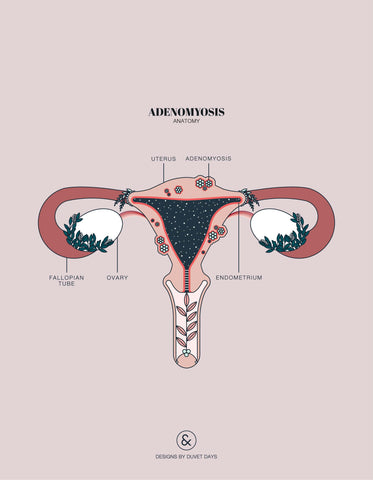
Adenomyosis
Adenomyosis is a condition similar to (and often experienced along with) endometriosis—sometimes considered a sister disease of endometriosis—where the endometrium sneaks into the walls of the uterus and begins to grow there as well. This can cause heavy, prolonged periods because more endometrium = more bleeding. It can also result in chronic pelvic pain, infertility, and pain during or after sex.
Adenomyosis can cause the uterus to feel tender, so it can be painful when it’s nudged around during sex—particularly during or after deep penetration.
While not much is known about adenomyosis, many of the options that can be used to treat painful sex associated with endometriosis can also be applied to adenomyosis.
Pelvic Floor Dysfunction
Pelvic floor dysfunction is when the muscles of the pelvic floor are not functioning optimally—meaning they may be too tight, weak, and/or lack range of motion—causing pain and/or problems with urination or bowel movements. Many of the conditions explained in the piece are types of or causes of pelvic floor dysfunction.
Pelvic floor physical therapy, lifestyle changes, medications, and sometimes surgery can all be used to treat the different kinds of pelvic floor dysfunction.
Interstitial Cystitis (IC)/Bladder Pain Syndrome (BPS)
Bladder Pain Syndrome is a mystery condition where there’s prolonged (more than six weeks) pain and what feels like pressure throughout the pelvis, often accompanied by a frequent and urgent need to pee. It may feel like you have a bladder infection when there is, in fact, no infection. While IC/BPS can affect anyone with a bladder, it is more likely to affect *women. Current estimates say IC/BPS affects 1 to more than 6% of *women in the U.S. but, numbers are growing as IC/BPS gains visibility.
IC/BPS can cause deep dyspareunia for a number a reasons, which are explained in greater detail by The Centers for Vulvovaginal Disorders. IC/BPS could be the cause of deep dyspareunia in and of itself; bladder pain and pressure + an object in the vagina = a recipe for ouch. This pain could also be caused by pelvic floor dysfunction, which is common among IC/BPS patients, or collision pain from bladder slings/mesh used to treat IC/BPS.
Physical therapy and lifestyle modifications (like abstaining from coffee) can help with symptoms including painful sex. Modifying positions (with or without Ohnut) and sticking to non-penetrative sex can also be useful for maintaining a happy, healthy sex life.
Uterine Fibroids
Fibroids are benign (non-cancerous) tumors that grow inside and on the uterus. Affecting up to 80% of U.S. *women by age 50, fibroids are particularly common among African Americans. Fibroids may cause long, heavy periods and bleeding between periods, increased cramping, lower back and pelvic pain, fatigue, and increased urination. But sometimes there won’t be any symptoms at all.
This can cause deep dyspareunia when large fibroids create pressure on the uterus, making penetrative sex uncomfy. Fibroids near the cervix can also lead to pain and discomfort.
Medications and surgical removal are most often what is used to treat fibroids. Getting a little creative with sex positions, incorporating Ohnut into your bedroom play, and opting for non-penetrative sex are also valid options that are less invasive, more cost-effective, and non-hormonal, but will not treat the source of the issue.
Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease is an infection in the uterus, fallopian tubes, and/or ovaries, often caused by an untreated sexually transmitted infection (STI). PID is common, affecting around 1 million people in the U.S. every year. For many, PID starts off as asymptomatic until the infection worsens. The symptoms then include longer, heavier, and more painful periods, fever/chills, tiredness, belly pain, and smelly vaginal discharge (not normal smelly, bad smelly).
PID can cause the pelvic organs to become inflamed, which can make having penetrative sex painful.
Good news! Making sure you are your partner(s) get tested for STIs and/or using condoms is a good way to prevent PID. And if you do happen to have an STI or PID, most cases can be treated with antibiotics.
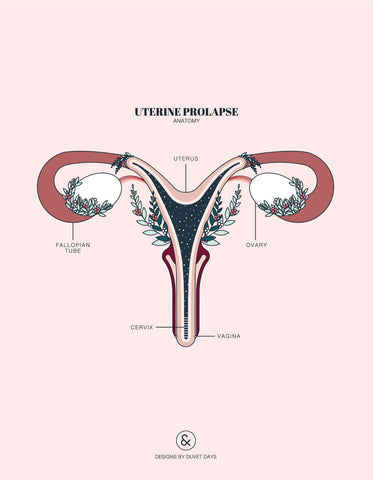
Uterine prolapse
Prolapse usually happens after vaginal birth when the uterus isn’t supported as well as it usually is by the pelvic floor muscles and ligaments. The uterus then begins to slip down towards or into the vagina. Postmenopausal *women are also particularly susceptible to prolapse because of pelvic floor dysfunction as a result of estrogen loss.
It is estimated that U.S. *women have an 11% lifetime risk of uterine prolapse. Mild prolapse usually doesn’t cause any symptoms, but more severe cases may mean a heavy feeling in the pelvis, tissue sticking out of the vagina, and urinary problems.
Unfortunately, painful sex is bound to follow when the uterus has decided to be bunkmates with the vagina.
Luckily, uterine prolapse is not inevitable! Enter: pelvic floor physical therapy. Pelvic floor PT can help to strengthen the pelvic floor so it can support those organs again like a champ.
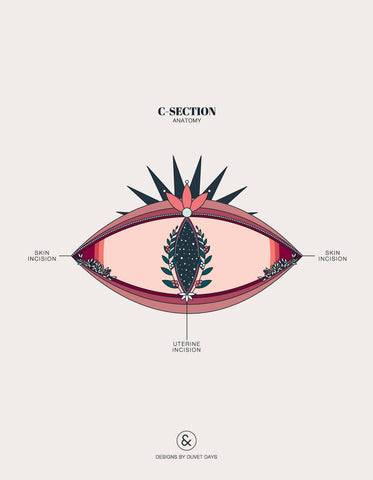
Scar Tissue / Pelvic Adhesions
Adhesions are bands of scar tissue that naturally form after trauma, inflammation, infection, or surgery. Commonly found on the pelvic organs and the bowel, they can bind these organs to other parts of the body, which can cause pain and impaired function. Because lots of things can cause adhesions (c-sections, endometriosis surgery, surgery to remove fibroids, pelvic inflammatory disease… the list goes on) and they’re often asymptomatic, it’s hard to determine how many people have pelvic adhesions. However, among those who have had surgery, trauma, infection, and/or inflammation in the pelvic region, the answer is… really common.
Adhesions can cause painful sex because they decrease the mobility of the organs they affect. Organs tend to squish around to compensate and make room during penetrative sex, which may mean pulling or stabbing pain when those organs aren’t as willing to move.
Preventing scarring is ideal, but not always possible. When scarring does occur and pain or discomfort is minimal, this can be controlled with medications or acupuncture. Physical therapy can also be useful for treating c-section scars or scarring post-abdominal surgery. The earlier you can treat a scar, the better.
When pain is more severe and cannot be addressed using other methods, adhesions can be removed via surgery—ideally of the minimally invasive variety because surgery itself can cause scarring.
Making adjustments in the bedroom—finding positions that feel good (which Ohnut can help with) or focusing more on non-penetrative sex—can be helpful too.
Cysts
Ovarian cysts are fluid filled sacs that may grow in or on the ovaries. In fact, cyst formation is a normal part of ovulation, and basically everyone with a period will form cysts. Each cycle, follicular cysts form, each housing a little egg inside it. Typically only one egg will mature to the point where it can be released, leading its surrounding cyst to rupture and freeing the egg (fun fact: some people can feel the cyst bursting!).
Ovarian cysts as a condition usually occurs when:
- The follicular cyst containing the egg never ruptures, causing the follicular cyst to continue growing. These will usually resolve on their own in a matter of months.
- The follicular cyst successfully ruptures and releases the egg, then forming what’s called the corpus luteum from the ruptured sac. Sometimes the sac will reseal itself and begin to fill up with fluid, creating a cyst. Again, these will usually resolve on their own, typically in a few weeks.
Usually cysts are asymptomatic, but when they do cause symptoms, that most often means pressure, bloating, and pain in the lower belly. These pains can be sharp or dull, and can be consistent or may come and go.
Ovarian cysts can cause painful sex because the ovaries may be bounced around a little during penetration, putting more pressure on the belly and pelvic organs or causing cysts to rupture.
Cysts will usually resolve themselves, but when they don’t, surgery and medications made to shrink the cysts are generally recommended for treatment. Again, if surgery or hormonal treatment aren’t viable and painful sex is the only concern, adjusting positions or exploring non-penetrative sex can be useful.
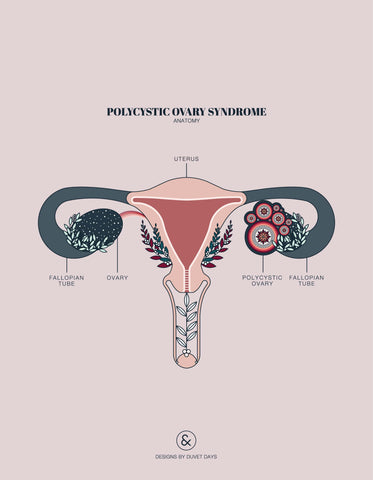
Polycystic Ovary Syndrome
In the case of Polycystic Ovary Syndrome, there may or may not be ovarian cysts (talk about a misnomer, right?). A common hormonal disorder, PCOS can cause irregular periods, heavy bleeding, excess hair growth, acne, weight gain, hair thinning and loss, development of dark patches of skin, and headaches.
This may cause deep pain during sex if there are large ovarian cysts (see above). Because irregular periods and problems associated with PCOS, like insulin resistance and diabetes, can lead to dryness and thinning of vulvar and vaginal tissue, people can experience vulvar pain and pain at the vaginal entrance during penetration. Experiencing this kind of pain (called superficial dyspareunia) can lead to the development of pelvic floor muscle dysfunction because this muscle group really like to guard in response to pain or anxiety. See the above section on pelvic floor dysfunction for more info!
Gender-Affirming Vaginoplasty
Gender-affirming vaginoplasty or “bottom” surgery is a procedure some trans women and trans femmes choose to have that involves the creation of a neovagina. Rates of dyspareunia among post-op trans women vary widely from 0 to almost a quarter. Bottom surgery is complex, and often results in a vagina that has varied elasticity and may be shorter than desired for deep penetration.
Painful penetration may be caused by lack of lubrication because some bottom surgery methods result in neovaginas that aren’t self-lubricating, which can lead to pain and discomfort during intercourse without added lubrication. Sex can also be painful if there is too much remaining erectile tissue surrounding the urethra, which can narrow the vagina during arousal.
Regular vaginal dilation is recommended—and essential—for the first few years, and then regular penetrative sex is usually enough to maintain the width of the vagina so sex is comfortable and pleasurable. If you’re unsure how to pursue dilation therapy, be sure to bring it up with your healthcare provider.
Cancer and cancer treatment
Many gynecological cancers cause deep dyspareunia; vaginal cancer, cervical cancer, ovarian/fallopian tube cancer, and uterine cancer symptoms can include pelvic pain and painful penetration.
Cancer treatment can also cause deep dyspareunia. Radiation therapy for any cancer of the pelvic organs (gynecological, colorectal, etc.) can result in decreased elasticity of the vagina, likely due to the formation of scar tissue, meaning the vagina is less flexible and therefore less able to accommodate penetration. A 2015 study found that 40% of gynecological cancer survivors they surveyed who were treated with radiation and had had sex recently experienced deep dyspareunia. Given there were hundreds of women that reported not having had sex in the past 6 months, deep dyspareunia caused by radiation therapy may be even more common in gynecologic cancer survivors.
Surgery can also be a cause deep dyspareunia. A variety of surgical treatment options for gynecological and pelvic cancers can result in a shortened or narrowed vagina. For instance, because the uterus and the cervix are removed during a radical hysterectomy, the vagina is shortened and some adjustments may need to be made to avoid painful penetration. Additionally, surgery can cause adhesions, the bands of scar tissue explained above.
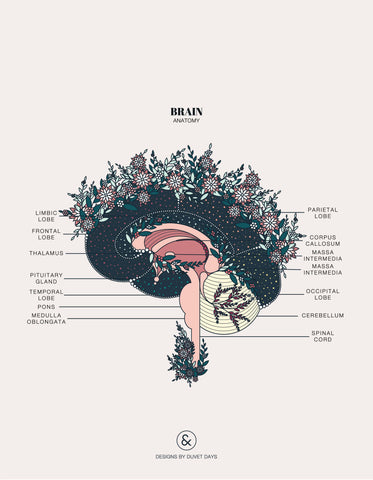
Stress / Trauma
The relationship between deep dyspareunia and stress/trauma is not well documented. However, the brain is a key sexual organ, so both stress and trauma can absolutely have a hand in deep pain or discomfort during sex.
Stress can make arousal difficult. This means the vagina might not tent or fully tent (lengthen), and there might not be enough lubrication. This can create friction, or pain when the back wall of the vagina is hit by the penetrating object.
Past or current trauma may also be a cause. If trauma has created feelings of anxiety, anticipation, or fear about sex, this can make being present and becoming aroused really hard. If sex is then painful, this can feed into a sexual pain/fear loop. When sex hurts, the brain remembers and can start to associate sex with pain—making it a scary experience. Being afraid isn’t a turn-on for most people and fear can increase the pain response, so subsequent sexual encounters can be painful, and so on.
Luckily, sex therapy and cultivating a mindfulness practice can be useful for disrupting the cycle of fear and pain, and helping manage stress and anxiety that can negatively impact sex. There may also be other underlying conditions, so it is always useful to talk to health practitioner like an OB/GYN or a pelvic floor PT.
Deep dyspareunia is a complicated phenomenon, an unwanted guest in your boudoir and you’re not quite sure how it got in. The list above is by no means exhaustive because painful sex has so many potential causes, both ones we know about and others we don’t. However, there are a growing number of treatment options for painful sex and conditions that cause it. We still have a lot to learn, but we do know that you deserve pleasure, and we want to help in any way we can.
*Not everyone who is a woman has a uterus, ovaries, fallopian tubes, a vulva, or a vagina. Not everyone who has a uterus, ovaries, fallopian tubes, a vulva, or a vagina is a woman.
Artwork: © Designs by Duvet Days / All Rights Reserved

Thank you for posting this helpful and informative page. I really appreciated having a comprehensive list of possible causes of pain “down there” and their descriptions all in one place.
J on
Very educating and helpful
MAIMUNA HASSAN SALEH on