Can HPV Cause Pain During Sex?
|
Time to read 7 min
|
Time to read 7 min
Human papillomavirus (HPV) is a VERY common virus with lots of different types. Some are sexually transmitted, and others are spread through regular ol’ human touching. Anywhere there are humans, there’s also HPV.
Fun fact: All warts are caused by HPV!
Yup, this pesky virus is the culprit of the warts you get anywhere on the body – head, shoulders, knees AND toes. These types of HPV can be spread through touching someone else’s wart or sharing objects (like wet towels), and ~thrives~ in places like common-use showers and pool decks.
In this article, we are talking specifically about the types of HPV that are spread through vaginal, anal, or oral sex, and may or may not cause warts.
“80 to 90% of vulva owners will get HPV at some point in their lifetime, so it is something that is super, super, super common,” says sexual health specialist Dr. Ashley Fuller, MD . We sat down with the Seattle-based OBGYN to discuss how HPV leads to conditions that require medical treatment, and why they may create pelvic pain.
Table of Contents
There are over 200 types of HPV. Most of the time, your immune system takes care of it on its own and you’ll have no idea you had it. Unfortunately, some types lead to genital warts, and others lead to vulvar and cervical cancer. There are two main categories, characterized by how likely they are to lead to cancer:
Low Risk HPV: genital warts
High Risk HPV: can lead to precancerous cells
If you're interested in the science of it:
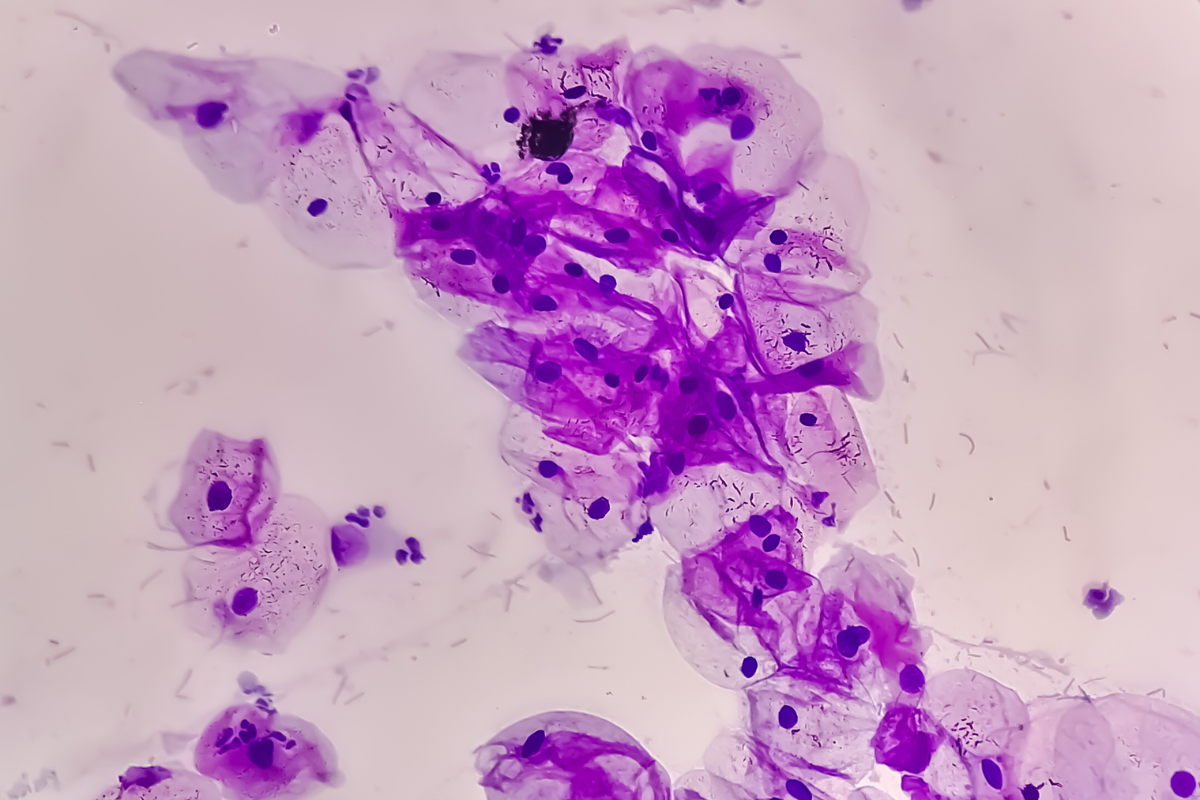
The virus infects healthy cells with its wonky DNA, making the cells replicate abnormally. Infection can create warts or precancerous growths (dysplasia), depending on the viral subtype.
Although HPV itself is unlikely to cause pain, medically necessary treatments and the psychological stress of having the virus can lead to pelvic pain.
“If you have genital warts, you can have itching [and] burning, and then you get a lesion that can be raised,” describes Dr. Fuller. These irregular-shaped lumps appear in one or multiple areas on the genitals/anus.
Genital warts are typically painless, but can cause discomfort, pain, or bleeding with friction or if the bumps are irritated (like during sex).
If you actively have warts or are being treated for warts, you can transmit them to a partner via skin to skin contact.
“A lot of times, the parts of the skin that have HPV are not necessarily those parts that can be covered by a condom, and you still can transmit it,” Dr. Fuller continues. “So, if you have active genital wart lesions, then I generally recommend having those treated or [it] could be passed onto a partner.”
If you’re interested in ~getting it on~ and the warts are not painful to the touch, consider clothed outercourse until the warts have been removed.
Topical creams stimulate the immune system to get rid of the virus, which creates temporary inflammation and irritation to the skin.
Cryotherapy (freezing the skin) causes small blisters to form, making the wart fall off.
Minor surgery is conducted in rare, extensive cases.
Most of these treatment options create some discomfort, but pain should resolve as the warts disappear. Doctors can also prescribe numbing agents for you while it heals.
“If you're sexually active, you're always swapping different strains of HPV back and forth, and sometimes you're unlucky enough to get one of the high risk ones,” says Dr. Fuller. It is SUPER important to get preventative pap smear screenings every 5 years!
If you receive an abnormal pap smear test result, doctors will assess how serious the progression is and closely monitor if your immune system clears it on its own, or conduct procedures to remove the abnormal cells.
Colposcopy: doctors go into the vagina with a microscope and take small clippings, or biopsies, of the cervix. This is a quick but uncomfortable procedure, feeling like little pinches on the cervix, so some doctors inject numbing agents and use medicine to stop the bleeding.
LEEP, or loop electrosurgical excision procedure: if the colposcopy shows more severe precancerous cells, the first layer of the cervix is shaved off with a hot wire loop. Ouch! Deep numbing agents are injected for this procedure. Even after healing, the cervix is thinner, and long-term scarring can make IUD insertion and dilation during labor more difficult.
The skin of the cervix is sensitive and can take up to a couple of months to heal after being poked and prodded. For some, resuming pleasurable sex happens fairly quickly. Unfortunately, some folks continue to experience painful penetration with cervical numbness and decreases in sexual and orgasmic satisfaction .
Deep penetration may further irritate the cervix, especially after a LEEP, so Ohnut depth-limiting rings could be helpful to eliminate the threat of pain. If you are having consistent pain after any of these procedures, be sure to let your gynecologist know.
Sometimes, precancerous cells are found on the vulva, similar to skin cancer on other areas of the body. The skin may change in appearance and become discolored or raised and lead to itching, burning, irritation, and vulvar pain.
Vulvar dysplasia/VIN is somewhat rare, and can be caused by HPV, or the skin conditions lichen sclerosus or lichen planus . VIN is categorized by how deeply the abnormal cells penetrate the layers of the skin:
VIN 1 is superficial and treated similarly to genital warts, with topical immune stimulating creams.
VIN 2 and 3 are deeper, and require surgical removal and suturing, and can cause scarring and pain after the procedure.
People that have undergone vulvar surgery for VIN may experience lasting pain and sexual dysfunction, especially with older age or larger affected areas.
Related Articles
Sexually transmitted infections are way more common than people tend to talk about, and HPV is the most common of them all. Experiencing HPV-related symptoms can be extremely distressing and can take a toll on one's mental health and sex life .
Many people experience shame after diagnosis, and Dr. Fuller remarks, “I always try to remind people of [how common HPV is], because so often there's a stigma around it, like they did something wrong … or a feeling of guilt that comes with getting it.”
An HPV diagnosis can reduce self-confidence and provoke fears of rejection from partners, spreading the virus, and pain from penetration. Desire may plummet as a result, especially if pain is involved.
Consistent pelvic pain can cause nerves around the vulva and vagina (there are a lot down there!), to become super duper sensitive, making the pain cycle more intense over time. Muscles may cramp more in response, and lead to conditions such as vaginismus . Dr. Fuller notices this association in her patients: “Maybe it started out as the skin, but then having the pain all the time made the muscles tight .”
If you feel burning, aching, or sharp pain during sex, it is important to speak to a doctor so they can help you understand the origin of your pain. Check out this pelvic pain assessment to help communicate your symptoms to a doctor.
HPV is not completely preventable and there is no cure if you’re one of those lucky duckies whose body can’t clear the infection. So if you have been diagnosed in the past, it’s possible to transmit it to partners even without active warts, or after treatment procedures. The good news is, there are measures you can take to prevent transmission and reduce the likelihood of catching other subtypes:
Communicate honestly with current or new partners.
Practice safe(r) sex with new partners (condoms, dental dams, outercourse—oh my!).
Get regular pap smears.
Get vaccinated!
The Gardasil vaccine is highly effective at preventing the most risk-associated forms of HPV , and is now approved to receive up until the age of 45. Dr. Fuller recommends that “even if you are in a monogamous relationship, I still recommend you get it, because there’s always life changing events that can happen.”
Anyone can get vaccinated, no matter the genitals! People with penises aren’t as prone to genital cancer, but can still get warts and other types of HPV-related cancer. Plus, getting vaccinated reduces the risk of passing on high-risk HPV types to partners.
Remember, there is nothing to be ashamed of, so you have every right to speak up for yourself and ask for numbing creams or pain meds during procedures or healing. Dr. Fuller reminds us that you are not alone if you are experiencing pain, and doctors and physical therapists are here to support you: “pain is a team sport, you need everyone involved.”
HPV is incredibly common
Genital warts and treatment for warts may cause short and longer term pain during sex
Tests and treatments for cervical dysplasia may cause some pain during sex
Vulvar dysplasia as a result of some HPV infections may cause long-term pain during sex
HPV isn't entirely preventable, but there are prevention and treatment options
